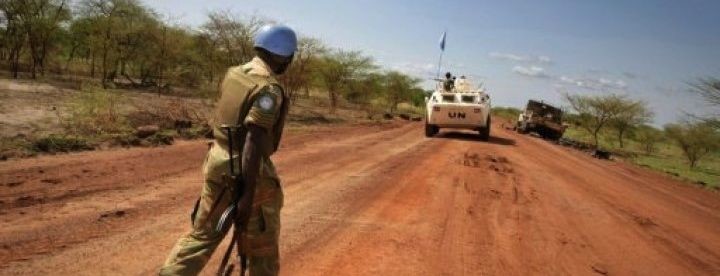
The United Nations Interim Security Force for Abyei (UNISFA) said it has completed the withdrawal of all peacekeepers and national monitors from its team sites in Tishwin and Abu Qussa/Wunkur after security conditions in the areas deteriorated.
In a statement on Friday, UNISFA said the decision followed an assessment that the security situation had become increasingly volatile and unpredictable, limiting the mission’s ability to protect its personnel and sustain operations at the sites.
The last convoy carrying peacekeepers, national monitors and equipment arrived in Abyei on March 6, marking the completion of the withdrawal.
UNISFA thanked Sudanese and South Sudanese authorities and the United Nations Mission in South Sudan (UNMISS) for supporting the process and helping ensure the safe movement of the convoy.
The departure from the two team sites of the Joint Border Verification and Monitoring Mechanism (JBVMM) follows last year’s evacuation of the mechanism’s logistics base in Kadugli after an attack on Bangladeshi peacekeepers.
The JBVMM monitors the Safe Demilitarized Border Zone (SDBZ), which was established in 2012 after Sudan and South Sudan agreed to create the buffer zone with support from UNISFA.
UNISFA said it remains committed to promoting peace and stability along the Sudan–South Sudan border and implementing arrangements agreed by the two countries.
The mission said the JBVMM headquarters has been temporarily relocated to Abyei while it continues to monitor the evolving situation and consult on future arrangements for carrying out the mechanism’s mandate.
UNISFA added that the safety and security of its peacekeepers remains a priority and that it will continue engaging with both governments on implementing the JBVMM mandate.
The United Nations Interim Security Force for Abyei (UNISFA) was established by the United Nations Security Council in 2011 to monitor and maintain peace in the disputed Abyei region along the border of Sudan and South Sudan.
The mission was created after the independence of South Sudan and amid tensions over the oil-rich Abyei area, which both countries claim.